Respiratory Medicine
In an emergency, please go to your nearest emergency department.
Specialist services
Most patients referred for a respiratory consultation will undergo lung function testing before their appointment to help with assessments.
These may include flexible bronchoscopy, endobronchial ultrasound, pleural procedures, cardiopulmonary exercise tests, bronchial challenge, and high-altitude simulation.
At RPH, Respiratory Medicine is a specialty providing a full spectrum of lung function tests for outpatients and inpatients with lung diseases.
Our physicians have special interests in asthma, lung cancer, respiratory infectious diseases, bronchiectasis, mycobacterial infections (including MAC), chronic obstructive pulmonary disease, interstitial lung disease, pleural diseases, and bronchoscopy.
Teams have been established across the health service to diagnose and treat Bronchiectasis, Interstitial Lung Disease, Asthma/ENT/Immunology, and Thoracic Oncology.
Our Clinics
| Clinic | Location | Day | Face to face | Telehealth? |
| General Respiratory | Desk 2&4, O Block, Goderich Street | Tuesday, Friday | ✔ | ✔ |
| Airways Disease | Desk 4, O Block, Goderich Street | Tuesday | ✔ | ✔ |
| Bronchiectasis | Desk 2, O Block, Goderich Street | Wednesday | ✔ | ✔ |
| Lung nodule | Desk 1, O Block, Goderich Street | Tuesday, Thursday | ✔ | ✔ |
| Pleural Diseases | Desk 1, O Block, Goderich Street | Monday | ✔ | ✔ |
| Rapid Access | Desk 1, O Block, Goderich Street | Tuesday, Friday | ✔ | ✔ |
| Telehealth | Telehealth Dept | Thursday | ✔ | |
| Interstitial Lung Disease | Desk 1, O Block, Goderich Street | Monday | ✔ | ✔ |
Note: If you have a concern for tuberculosis, contact the Anita Clayton Centre.
Sleep clinic: RPH does not have an outpatient sleep service or a sleep study laboratory. Public patients being referred for sleep disordered breathing can be referred to Fiona Stanley Hospital, SJOG Midland, Sir Charles Gardner Hospital or Joondalup Health Campus.
Why do we measure lung function?
- It tells us how your lungs are working and helps in ongoing monitoring
- It helps in the diagnosis of different lung diseases
- It helps for the planning of your treatment.
Big blow test (Spirometry)
Spirometry is a test used to see if there is any narrowing in your airways. Lung conditions like asthma can cause shortness of breath by narrowing the airways, so that airflow through the lungs is reduced. In this test, we measure how fast you can empty your lungs and how much air you can blow out.
The process:
- Take a big deep breath in
- Blow out as hard and fast as you can until you are empty
Giving Medication (Bronchodilator)
To see if your airway narrowing can be reversed, you may be asked to repeat the spirometry test after breathing in a reliever drug such as Ventolin.
How big are your lungs? (Plethysmography)
We do lung volume measurements to see how much air is in your lungs when you take a big breath in to the top. The “Box” is a chamber similar in size to a telephone booth, which you sit in with the door closed. We measure changes in pressure as you pant, which relates to lung volume.
The process:
- Breathe normally with your hands on your cheeks
- A shutter will close, blocking the air
- Gently pant (suck and blow) against the closed shutter keeping your lips tight around the mouthpiece
How well does oxygen go into your body? (Diffusing Capacity)
The diffusing capacity test (or DLCO) looks at your gas exchange (how easily the air you breathe in travels into your lungs and into your bloodstream). We use this information to assess the severity of lung conditions such as emphysema or pulmonary fibrosis.
The process:
- Breathe out until you are empty
- Take a big breath in of a special gas mixture
- Hold your breath for 10 seconds
- Breathe out
6 Minute Walk Test
The six-minute walk test looks at any impairment you may have when you go about your daily tasks. The test can help us to see if you need oxygen at home.
The process:
- Wear a monitor (in a sling) so that we can see your oxygen and heart rate during the test
- Walk up and down a hallway as many times as you can in 6 minutes
Do you need extra oxygen to fly? (High Altitude Test)
When you fly in a plane, there is a lower level of oxygen in the air you breathe. If you have a lung or heart condition and are planning to fly, you may become unwell in this low oxygen environment.
A high altitude simulation test will allow us to work out if you need extra oxygen on board the aircraft. During the test, should your oxygen levels fall too low, we will give you extra oxygen. Based on your oxygen levels throughout the test, we will see what level of extra oxygen you may need for your flight.
The process:
- Sit with a mask positioned over your nose and mouth
- Breathe normally, you will be breathing in a lower level of oxygen (equivalent to when you are on the plane) and your oxygen levels will be monitored
- You will also be asked to do a small stepping exercise to see if this effects your oxygen levels (for example if you need to get up and go to the toilet during your flight)
Royal Perth Hospital have developed instructional lung function videos to help patients (in particular Aboriginal patients) and healthcare professionals understand the requirements for lung function tests.
Big blow test (Spirometry)
How big are your lungs? (Plethysmography)
How well does oxygen go into your body? (Diffusing Capacity
Do you need extra oxygen to fly? (High Altitude Test)
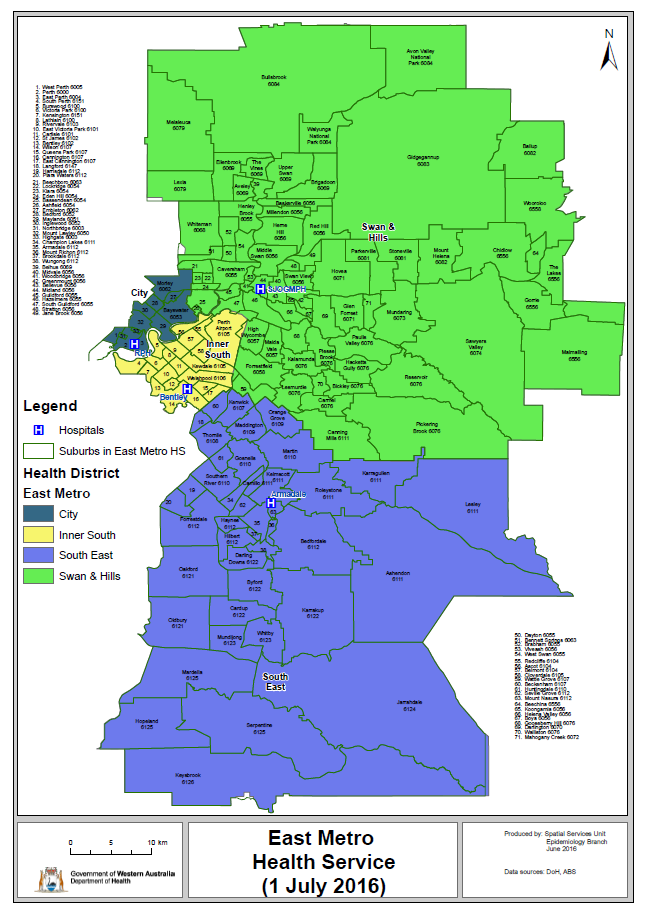 For your information, the catchment map (PDF 400KB) outlines the suburb catchment areas for East Metropolitan Health Service (EMHS). The country areas that flow to EMHS are Kimberley, Pilbara and Wheatbelt.
For your information, the catchment map (PDF 400KB) outlines the suburb catchment areas for East Metropolitan Health Service (EMHS). The country areas that flow to EMHS are Kimberley, Pilbara and Wheatbelt.
Referral to a hospital for assessment and/or treatment is based around multiple criteria. These include:
- Place of residence – most hospitals have catchments to help service people closer to home. For country patients, the residence of family with whom they will reside whilst attending appointments can be taken into consideration.
- Age – children are only treated by some hospitals.
- Hospital location of specialty services – some conditions need designated specialist services that are not available at all hospitals.
For Country patients please consider a local service, view resources on the AHCWA MAPPA website (external link)
Use this information to guide urgent referrals to the hospital servicing your patient's postcode.
Inform your patients of these criteria when you are referring them for public hospital services.

