Preventing Infections in Our Health Service
The prevention and control of infections across East Metropolitan Health Service is an integral part of safety and quality improvement.
Throughout this section we provide auditing results and statistics relating to healthcare associated infections (infections people acquire while being cared for in our healthcare facilities) and our hand hygiene compliance.
Infections people get while being cared for in a healthcare facility are known as healthcare associated infections (HAI).
The most common types of infection acquired in hospitals are:
- bloodstream infection
- urinary tract infection (UTI)
- pneumonia (lung infection)
- wound infection.
For a patient, a HAI can result in:
- illness
- an extended stay in hospital
- a slower recovery
- increased stress
- lower morale.
While HAIs are costly to patients, hospitals and the community, financial impact is just one factor which needs to be considered when addressing the issue, with the stress caused to the patient also a key consideration. While they can occur in any healthcare setting, effective infection prevention and control can significantly reduce the infection rate. Patients, visitors and staff all play a role in reducing HAIs.
About Staphylococcus aureus bloodstream infections (SABSIs)
An important cause of common HAI is Staphylococcus aureus (S. aureus), also known as ‘Golden Staph’. It is a type of bacteria often found on the skin of healthy people and is usually harmless. In hospitals, transmission is most commonly via the hands of healthcare workers.
Most cases can be treated by antibiotics; however, there are more serious antibiotic-resistant strains. It is estimated that contracting a healthcare-associated S. aureus bloodstream infection whilst in hospital, can be life-threatening or cause serious harm in 20 to 35 per cent of cases.
Measuring hospital acquired bacteraemia
The rate of healthcare associated S. aureus bloodstream infections (SABSIs) is measured by counting the number of infections and dividing by the number of beds occupied by patients each day (occupied bed days) over a three-month period. For an infection to be considered healthcare-associated there must be no evidence that it was present or developing at the time of hospital admission.
The definition of a SABSI was developed by the Australian Commission on Safety and Quality in Health Care.
The nationally agreed benchmark set under the National Healthcare Agreement (NHA) is no more than 2.0 cases of healthcare associated S. aureus bloodstream infection per 10,000 days of patient care for public hospitals in each state and territory.
WA Health has set a benchmark of less than or equal to 1.0 healthcare associated S. aureus bloodstream infection per 10,000 bed days.
To minimise the risk of patients getting a preventable infection, each EMHS hospital has a surveillance program through which they closely monitor infection rates and evaluate the effectiveness of strategies used to prevent and control SABSIs. Surveillance data is reported throughout all levels of the health service to support good decision-making in the prevention of SABSIs.
All identified cases of infection undergo review by infection control specialists to ascertain anything that the service could have done to prevent the infection. Given the complexity of health care and patients seen, not all cases of infection will be considered preventable.
How do we measure up
The graph below shows the combined healthcare associated bacteraemia rate for Royal Perth Hospital.
Chart: Healthcare-associated S. aureus bloodstream infection rate per 10,000 bed days.
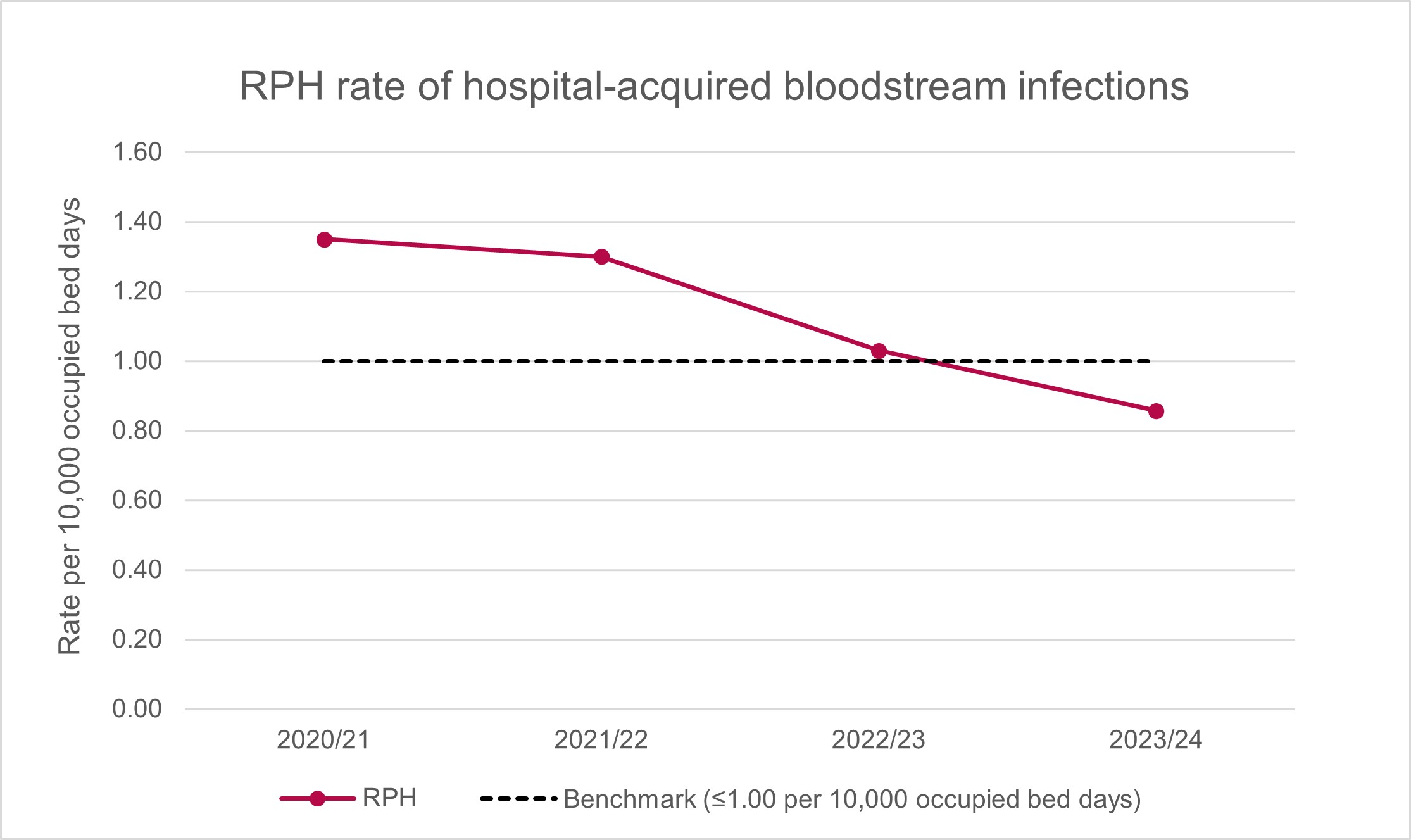
What the figures mean
The graph shows the overall rate of S. aureus bloodstream infection across RPH by financial year.
The benchmark is less than or equal to 1.0 hospital-acquired bloodstream infection per 10,000 occupied bed days. A rate lower than the benchmark is desirable.
The rate of S. aureus bloodstream infections at RPH has been trending towards the benchmark, with the most recent financial year being better than the benchmark. RPH continues to monitor, review and identify strategies towards greater prevention of infection.
Good hand hygiene (washing or decontaminating hands with soap and water or an alcohol-based hand rub) is an important part of good patient care.
Hand Hygiene Australia (HHA) describes improving hand hygiene among healthcare workers as the single most effective intervention in reducing healthcare-associated infections (HAI) in Australian hospitals. The aim is for healthcare workers to perform hand hygiene correctly at every opportunity, for example, before and after touching a patient.
The National Hand Hygiene Initiative (NHHI) was implemented to develop a national approach to improving hand hygiene and monitor its effectiveness. Although not nationally comparable, hand hygiene information helps to drive quality improvement in hospitals.
Measuring hand hygiene compliance
Hand hygiene is measured by observing a specified number of ‘moments’ before and while caring for patients:
- Moment 1: Before touching a patient
- Moment 2: Before a procedure
- Moment 3: After a procedure or body fluid exposure risk
- Moment 4: After touching a patient
- Moment 5: After touching a patient’s surroundings.
The estimated hand hygiene rate for a hospital is a measure of how often hand hygiene is correctly performed (as a percentage). It is calculated by dividing the number of observed hand hygiene ‘moments’ where proper hand hygiene was practiced in a specified audit period, by the total number of observed hand hygiene ‘moments’ in the same audit period and multiplying by 100. The rate is rounded to one decimal place.
Hand hygiene data is provided by State and Territory health services for public hospitals and by individual private hospitals. The data is derived from audits of hand hygiene ‘moments’ conducted up to 3 times per year through the National Hand Hygiene Initiative. Audits are performed by individuals who have undergone HHA auditor training.
The Australian Commission on Safety and Quality in Health Care recommends a benchmark hand hygiene rate of 80 per cent.
How do we measure up
The graph below shows the combined hand hygiene compliance rate for Royal Perth Hospital.
Chart: Royal Perth Hospital hand hygiene results for audit periods.
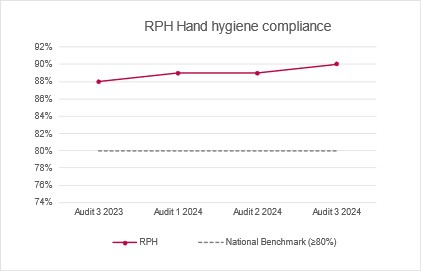
What the figures mean
The graph shows the hand hygiene compliance rate for RPH for the last four audit periods. A rate higher than the benchmark is desirable.
In the last four audit periods, RPH has consistently achieved greater than the benchmark of 80% compliance.
Surgical site infections (SSI) is one of the most common complications associated with surgery and every patient who undergoes surgery is at risk of acquiring an infection. A patient who develops a SSI will often have a longer hospital stay or be readmitted, require antibiotics to treat the infection, and sometimes require further surgery.
A surveillance program that includes monitoring of SSIs can have an immediate and prolonged impact on reducing infections. WA hospitals share this information with their clinicians and hospital executives and use this information to support improved compliance with infection prevention strategies and to initiate practices to further improve patient outcomes.
Measuring surgical site infections for selected surgical procedures
The rate of surgical site infection is measured by counting the number of patients with an infection from the surgical procedure during a set period and dividing by the total number of patients who have undergone the surgical procedure during the set period.
The two selected surgical procedures that are measured are:
- Primary Hip Arthroplasty
- Primary Knee Arthroplasty
Primary hip arthroplasty
How do we measure up
The graph below shows the surgical site infection rate for the primary hip arthroplasty procedure for Royal Perth Hospital.
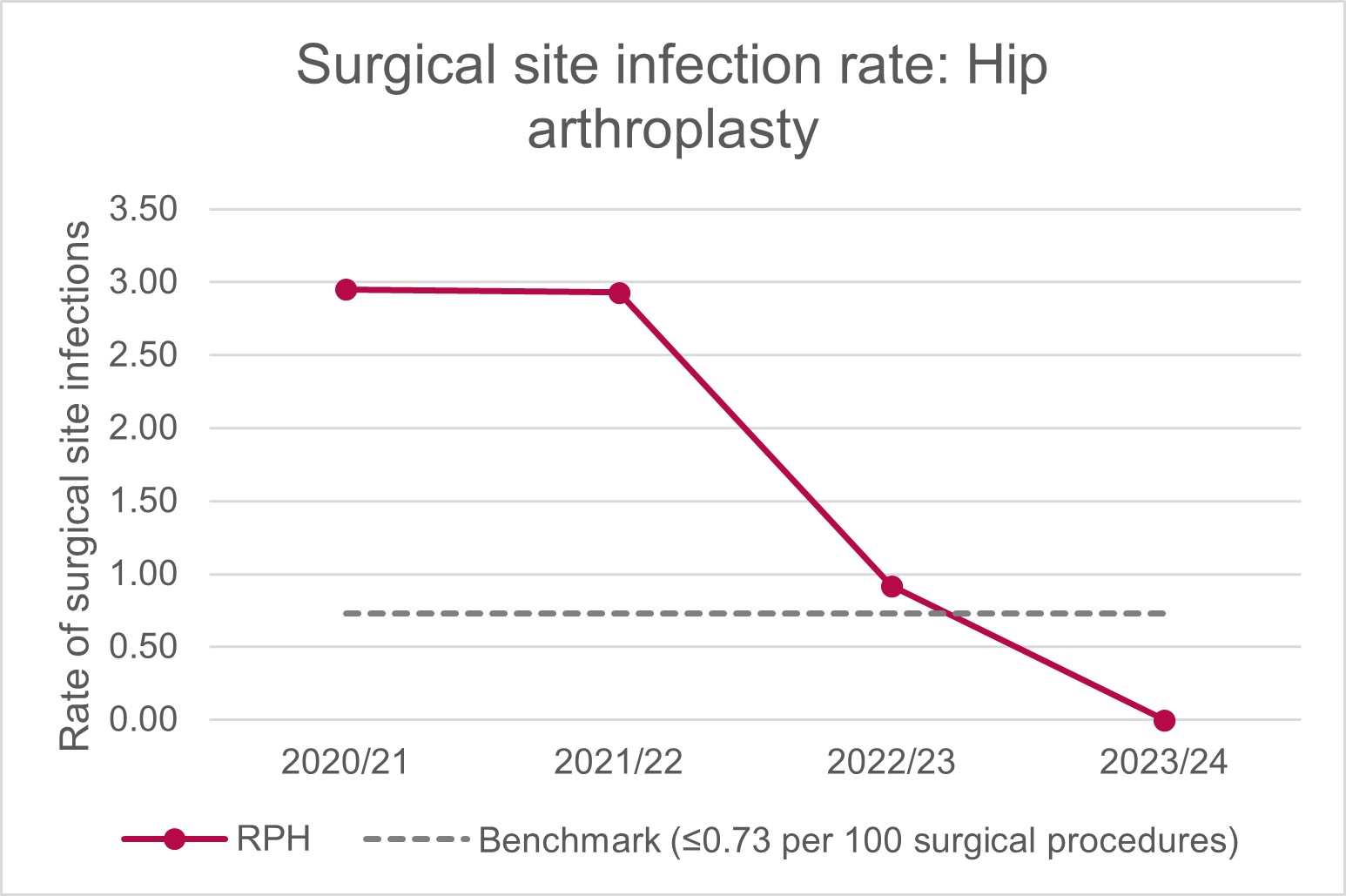
What the figures mean
The graph shows the overall rate of surgical site infection for primary hip arthroplasty for RPH by financial year.
The benchmark is less than or equal to 0.73 infections per 100 surgical procedures. A rate lower than the benchmark is desirable.
The rate of surgical site infection has been above the benchmark for three years of the past four years. RPH continues to monitor, review and identify strategies towards greater prevention of infection.
Primary knee arthroplasty
How do we measure up
The graph below shows the surgical site infection rate for the primary knee arthroplasty procedure for Royal Perth Hospital.
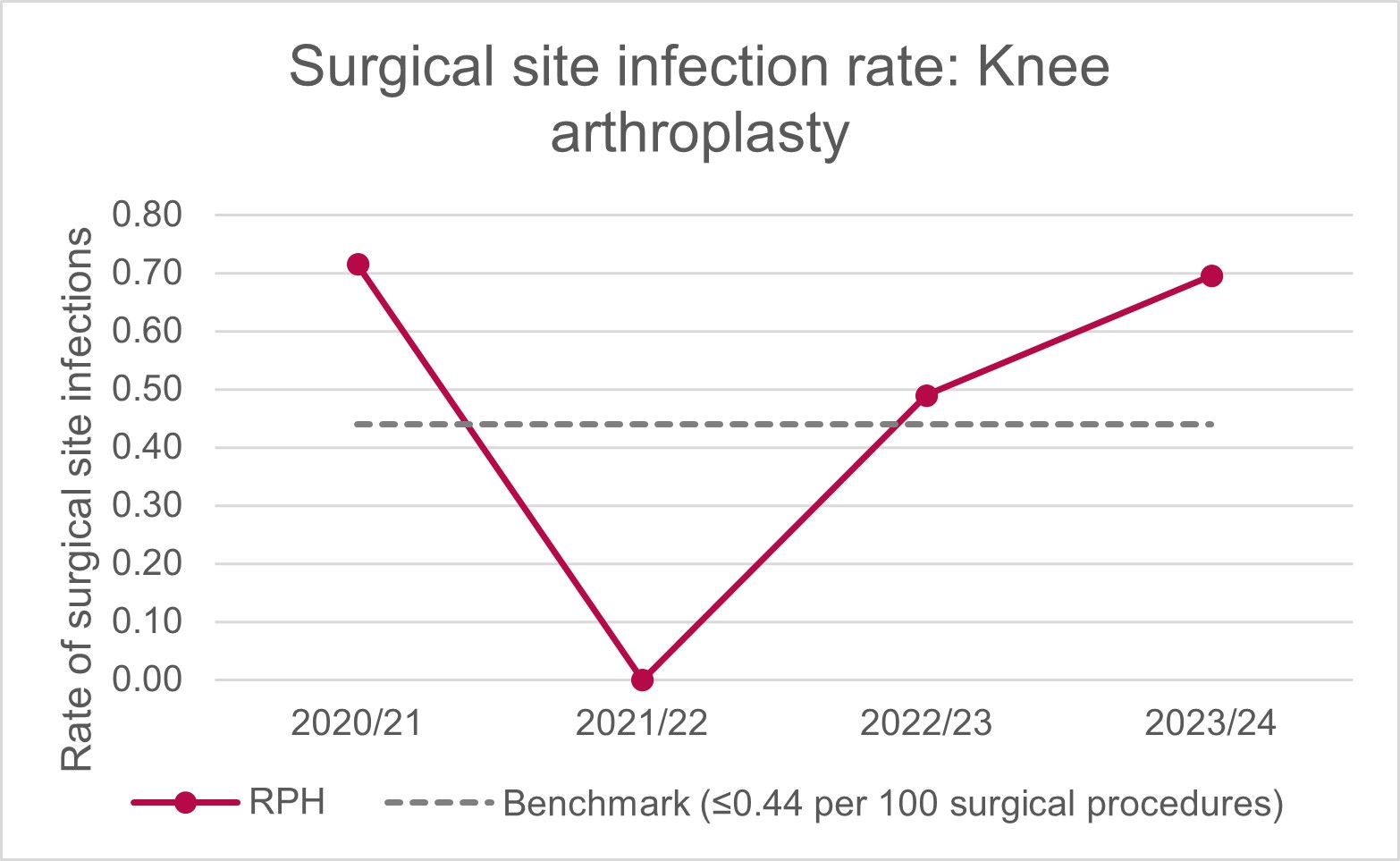
What the figures mean
The graph shows the overall rate of surgical site infection for primary knee arthroplasty across EMHS public hospitals by financial year.
The benchmark is less than or equal to 0.44 infections per 100 surgical procedures. A rate lower than the benchmark is desirable.
The rate of surgical site infection has been above the benchmark for three of the last four years. RPH continues to monitor, review and identify strategies towards greater prevention of infection.

