Cough
Disclaimer
These guidelines have been produced to guide clinical decision making for general practitioners (GPs). They are not strict protocols. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
|
Introduction
Chronic cough is defined as a daily cough that persists for more than 4 weeks1,2. It is important to differentiate between a chronic cough and recurrent cough from serial respiratory tract infections. Chronic cough should prompt further assessment to establish the underlying diagnosis.
Please refer to Clinician Assist WA-Persistent Cough in Children for more information3.
Assessment
- Age-appropriate cough history including:
- Onset
- Quality (in particular “dry” vs “wet” cough)
- Pattern
- Triggers
- Associated features of concern (e.g. dyspnoea, haemoptysis, poor growth, reduced exercise tolerance, swallowing difficulties and choking history)
- Other related factors including:
- Atopy
- Relevant family history
- Environmental factors (including tobacco smoke exposure)
- Perinatal factors (e.g. prematurity, neonatal respiratory distress)
- Explore parental concerns and expectations.
- Features of concern on physical examination including:
- Auscultatory findings (e.g. persistent wheeze or crepitations, differential breath sounds)
- Digital clubbing
- Chest wall deformity (e.g. asymmetrical chest wall, pectus carinatum)
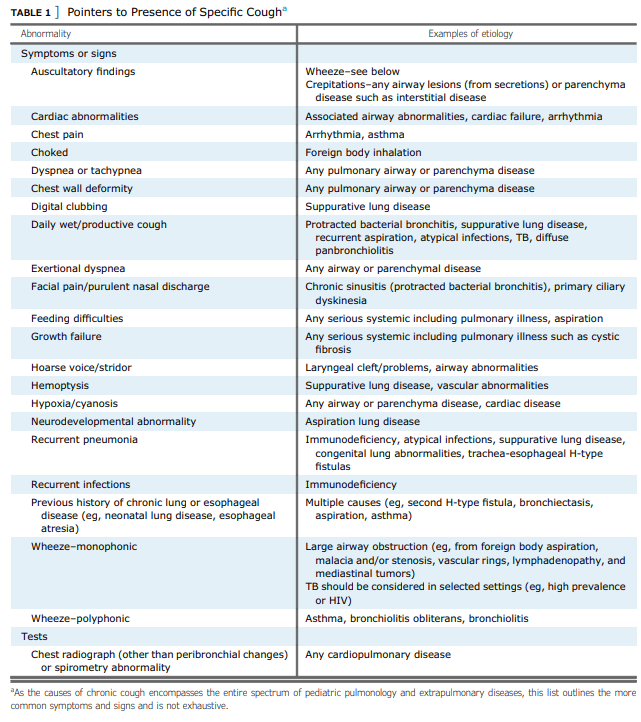
Specific Features of Concern
- Presence of specific cough pointers may indicate aetiology of chronic cough – refer to the following table2:
Broad differential diagnoses (list not exhaustive):
- Dry cough
- Prolonged post-infectious cough (consider pertussis or mycoplasma)
- Asthma (unlikely if no wheeze or dyspnoea)
- Rhinitis or rhinosinusitis
- Somatic cough disorder or tic cough
- Moist cough
- Protracted bacterial bronchitis (PBB), the most common cause of chronic wet cough in children
- Aspiration syndromes including foreign body inhalation and chronic/feed-related aspiration
- Cystic fibrosis
- Bronchiectasis
Pre-referral investigations
- Chest x-ray
- Spirometry if able (consider in children aged > 6years)
- Direct referral for spirometry only at PCH Respiratory Laboratory without clinical review is available
- Sputum culture in children with wet cough, who can produce a sample
Pre-referral management
- If suspected PBB (chronic wet cough with no pointers to alternative diagnosis):
- Treat with a 2 to 4-week course of oral antibiotics until resolution of wet cough.
- Suggest empirical treatment with broad spectrum antibiotic such as amoxicillin/clavulanic acid 25mg/kg (max 875mg amoxicillin component) twice a day
- If penicillin-allergic, consider azithromycin or co-trimoxazole
- Refer if chronic wet cough does not resolve with antibiotic treatment or recurs
- If non-specific dry cough with normal chest x-ray +/- spirometry and no cough pointers, it may be appropriate to adopt a watchful waiting approach. Evaluate exposure to tobacco smoke and other pollutants, as well as reviewing parental expectations and concerns.
- Consider blood tests for respiratory serology (pertussis and mycoplasma) and screening for immunodeficiency and/or atopy
- If dry cough persists after another 2-4 weeks, consider trial of therapy with inhaled corticosteroids (e.g. fluticasone propionate 100mcg twice a day)
When to refer
- When pointers (see Table 1) indicate underlying disease
- Recurrent (3 or more) episodes of PBB or pneumonia
- Suspected PBB with wet cough not responding to prolonged 4-week course of oral antibiotics
- Suspected aspiration, cystic fibrosis, or bronchiectasis
- Refractory asthma
- Non-resolution of a non-specific cough
- Failure to thrive with potential respiratory cause
- Persistent crepitations +/- dyspnoea
- Presence of specific cough pointers
- Significant and persistent abnormalities in chest x-ray and/or spirometry
If significant concerns such as hypoxia or suspected inhaled foreign body, please discuss with the on-call PCH Respiratory team and place urgent referral, as child likely to require same-day review.
How to refer
- Routine non-urgent referrals from a GP or a Consultant are made via the Central Referral Service
- Routine non-urgent referrals from private hospitals are made via the PCH Referral Office (Fax: 6456 0097 or email PCH.Referrals@health.wa.gov.au)
- Urgent referrals (less than seven days) are made via the PCH Referral Office. Please call Perth Children’s Hospital Switch on 6456222 to discuss referral with Respiratory doctor on-call.
Essential information to include in your referral
- Detailed medical history including concerning features on history and examination
- Previous treatment and response
- Results of chest x-ray, spirometry and/or any blood tests
| Reviewer/Team: |
Respiratory and Sleep Medicine Department
|
Last reviewed: |
Nov 2022 |
|
|
Review date: |
Nov 2025 |
This document can be made available in alternative formats on request for a person with a disability.