Femoral nerve block
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer
|
Aim
To guide Emergency Department (ED) staff in the use of femoral nerve block.
Background
A femoral nerve block is a quick, easy, effective and safe method of providing analgesia to the child with a femoral shaft fracture as the femoral nerve (L2-L4) innervates the shaft and periosteum of the femur.
Anatomy
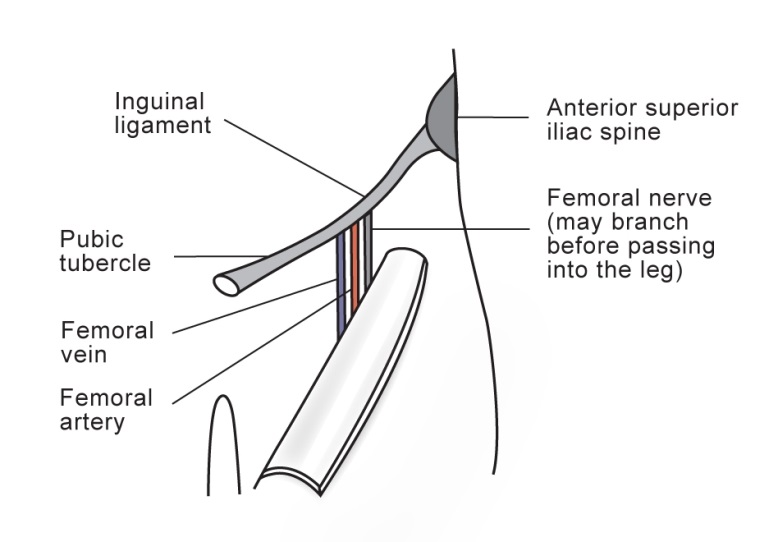
- The inguinal ligament extends from the pubic tubercle to the anterior superior iliac spine
- At its mid point, the femoral vein, artery and nerve pass beneath it
- The femoral vein lies medial, the artery in the middle and the nerve lateral
- A useful acronym is: NAVY = Nerve, Artery, Vein, Y fronts (!)
Principles
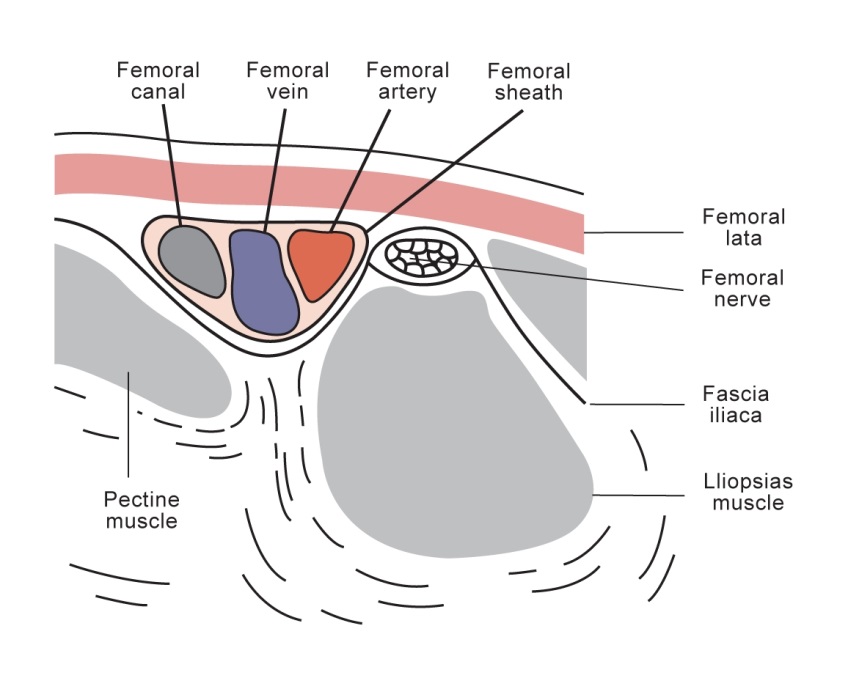
- The femoral nerve lies in its own tissue plane, is quite superficial (usually 1-2 cm deep; never more than 3cm deep, even in older children) and is separated from the femoral vessels by the fascia iliaca.
- Exact identification of the nerve position isn’t necessary.
- Local anaesthetic injected into the correct plane (just deep to the fascia iliaca) will result in effective nerve block by diffusion of anaesthetic, without the vascular compartment being affected.
Note: ultrasound guided femoral nerve blocks can be done if you are appropriately trained.
Pre-procedure
Indications
Requirements
- The patient needs to be able to cooperate with injections and hold still for the procedure intended.
- A clear explanation of the procedure needs to be provided to the patient.
- Risks need to be explained.
- Pain as the injection is made.
- Nerve block might not work.
- Bruising and bleeding at the site of injection.
- Ensure the patient is in the appropriate treatment area.
Preparation
Safety
Blocks should only be performed by or under direct supervision of appropriately trained staff.
STOP BEFORE YOU BLOCK3
Confirm
- Correct patient
- Correct side / site
- Correct indication
- Drug choice and dosage
- Equipment
- Pre-procedure vital signs
- Consent – written consent gold standard, verbal consent must be clearly documented
Contraindications
- Known local anaesthetic allergy
- Skin trauma or infection at site of injection
- Abnormal motor or sensory neurological findings prior to procedure
- Refusal of consent
Observations
The following are standard of care for major nerve blocks3:
- Cardiac monitoring
- Oxygen saturation monitoring
- Frequent and regular blood pressure recordings
- IV access is suggested in case of inadvertent intravascular delivery of local anaesthetic with resulting toxicity, however a senior clinician may decide to proceed with the nerve block before an IV is placed in order to control pain in a timely manner.
Signs of local anaesthetic toxicity include
- Central Nervous System (CNS) effects
- Perioral numbness / tingling
- Agitation
- Seizure
- Cardiovascular effects
- Hypotension
- Tachycardia
- Dysrhythmia
- Arrest
Refer to ED Guideline Lipid infusion for local anaesthetic toxicity, for management of toxicity.
Equipment
- Sterile gloves
- Dressing pack
- Skin cleaning antiseptic solution
- Needle: 23 gauge (blue) short bevel needle or 25 gauge (orange) in an infant
- Ultrasound (if using ultrasound guided technique)
Medications
- The lowest dose which provides sufficient analgesia should be used
- Higher volume of low concentration local anaesthetic (LA) is preferred to low volume of a high concentration LA
- High volume will cover a greater surface area of the nerve and facilitate better blockade
- The dose and time of administration should be clearly documented on the patient’s medication chart.
- Consider topical local anaesthetic e.g., lidocaine (lignocaine) with prilocaine (EMLA®) application over injection site.
Ropivacaine hydrochloride4,5,6
- Concentrations
- PCH ED stocks ropivacaine 0.75%
- Dose
- 1.5 mg/kg (0.2 mL/kg of ropivacaine 0.75%) for children ≥ 6 months.
- Published safe dosage of local anaesthetics for peripheral nerve blocks in children younger than 6 months is lacking.
- To avoid excessive dosage in obese patients, dose should be calculated on the basis of ideal bodyweight.8
- There is 7.5 mg of ropivacaine in every 1 mL of ropivacaine 0.75%.
- This can be diluted to a larger volume using sodium chloride 0.9%.
- Onset
- Duration
Multiple Blocks
- Total maximal dose should be calculated and divided equally if bilateral blocks being considered or local anaesthetic has been used for any other indication.
- The dose can be diluted to a larger volume with sodium chloride 0.9%.
- A more dilute dose will have slower onset of action but still provide adequate analgesia.
Repeated Blocks
- Blocks should not be repeated within 6 hours.
- If analgesia is inadequate consider systemic analgesia.
Procedure
- Principles of asepsis should be observed throughout procedure.
Ultrasound (US) Guided Nerve Block7
- US guided femoral nerve block represents the gold standard technique.
- US increases block success and minimises potential complications.
- US guided regional anaesthesia requires appropriate training which is beyond the scope of this guideline.
Positioning and technique
- Position the patient lying on a bed with the area appropriately draped and prepare with aseptic technique.
- Clean the skin with antiseptic solution.
- Identify the site of injection again (see above in Anatomy section).
- Keeping one finger on the femoral artery 0.5 – 1 cm below the inguinal ligament, insert the needle perpendicular to the skin, 0.5 – 1 cm lateral to the artery.
- The plane in which the nerve lies can be found by feeling a ‘pop’ or loss of resistance twice, first when the needle passes through the fascia lata, and then as it passes through the fascia iliaca.
- Note that the nerve is fairly superficial (1-2 cm) and most failed blocks are due to injecting too deep.
- Aspirate to make sure the needle is not in a blood vessel.
- Inject the local anaesthetic slowly, while frequently aspirating briefly to make sure the needle tip has not migrated into a vessel.
- Some authors describe injecting in a fan shaped pattern around the nerve, however this is not necessary since local anaesthetic injected anywhere under the fascia iliac will diffuse to the nerve and result in a successful nerve block.
- Place a pressure dot dressing over the injection site.
References
- Textbook of Paediatric Emergency Medicine 3rd Edition Cameron P, Browne GJ, Mitra B, et al (2018) Publisher: Elsevier Edition updated
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
- ANZCA professional document PG03(A) Guideline for the management of major regional analgesia 2014
- Ropivicaine. Australian Medicines Handbook (AMH) [Last modified July 2023. Cited October 2023] Available from: Ropivacaine - Australian Medicines Handbook (health.wa.gov.au)
- Ropivacaine – Dosing/Administration. IBM Micromedex 2022. Updated: 1 February 2022. Cited: 22 March 2022. Available from: Drug Result Page - In-Depth Answers - Dosing/Administration - Comparative Efficacy (health.wa.gov.au)
- Ropivacaine - Australian Injectable Drugs Handbook 8th Edition, Last Updated: 24 Nov 2021, Cited: 5 Jan 2022. AIDH - ROPIVACAINE (health.wa.gov.au)
- www.nysora.com/techniques/lower-extremity/femoral/femoral-nerve-block
- Ropivacaine hydrochloride BNF for Children. Medicines Complete. [Last updated 9 December 2019. Cited: 12 December 2023] Available from: MedicinesComplete — CONTENT > BNF for Children > Drug: Ropivacaine hydrochloride (health.wa.gov.au)
- Ropivacaine: Drug Information UpToDate [Cited 12 December 2023] Available from: Ropivacaine: Drug information - UpToDate (health.wa.gov.au)
| Endorsed by: |
Drug & Therapeutics Committee |
Date: |
Jan 2024 |
This document can be made available in alternative formats on request for a person with a disability.